The Importance of Patient Monitoring in the Post Anesthesia Care Unit
07-18-2024

Ensuring patients are safe after undergoing anesthesia is necessary to achieving positive outcomes from surgical procedures. During surgery, patients are vulnerable to complications from anesthesia that need to be monitored closely once in the post-operative phase. Implementing robust safety measures, from the Operating Room to the Post Anesthesia Care Unit is crucial. This requires meticulous planning, continuous monitoring, and immediate intervention to address any emerging issues. By prioritizing comprehensive safety protocols and utilizing advanced technologies, healthcare professionals can minimize risks, improve recovery times, and ultimately enhance the overall quality of care.
What is a Post Anesthesia Care Unit?
\r\n\r\n"}}" id="text-9d1cdc7a2f" class="8f00b2 cmp-text">
The Post Anesthesia Care Unit (PACU) is a care unit focused on the recovery of patients immediately following surgical procedures where anesthesia is administered. The PACU serves as a place where patients are carefully monitored to ensure they recover safely from their surgical procedure and the effects of anesthesia without complications. Within the PACU, attentive patient care is paramount in shaping patient outcomes and determining a patient’s length of stay, thus making effective patient monitoring technology essential within this specialized environment.
Why Patient Monitoring in the PACU is Vital
Continuous patient monitoring is a vital part of caring for patients in the PACU because the immediate postoperative period is when patients are at the greatest risk for respiratory and cardiovascular complications during recovery from surgery and anesthesia.1 PACU nurses are tasked with stabilizing patients postoperatively so they can either be transferred to an inpatient unit or be discharged to go home. This includes utilizing patient monitoring technology to accurately assess vitals, respiration rates, SpO2 levels, and other critical changes that alarms may signal. Discharging a patient too early can lead to poor patient outcomes, making it essential that nurses and surgical team members use a systematic approach to caring for patients during the post anesthesia period to ensure a safe recovery and discharge.2
Best Patient Monitoring Practices in the PACU
\r\n\r\n
Phase I is when patient monitoring is most critical for determining patient postoperative recovery status and assessing the patient’s stability for safe transition to phase II. To ensure patients are ready for the next phase of care, PACU nurses must monitor for the following events:
\r\n"}}" id="text-ea8c11aac3" class="8f00b2 cmp-text">A patient’s care in the PACU occurs in two phases: post anesthesia phase I and post anesthesia phase II. In phase I, nurses are responsible for providing routine, life-sustaining care to ensure the patient is recovering properly and is not at risk for postoperative morbidity or mortality. During phase II, PACU nurses’ main focus is to prepare the patient for discharge to home or for transfer to another unit, such as the Medical-Surgical Unit (MedSurg) or the Intensive Care Unit (ICU) for extended care.
Phase I is when patient monitoring is most critical for determining patient postoperative recovery status and assessing the patient’s stability for safe transition to phase II. To ensure patients are ready for the next phase of care, PACU nurses must monitor for the following events:
Enhancing PACU Safety with Advanced Patient Monitoring Technology
Patient monitoring systems that easily integrate into existing hospital workflows can help enhance patient care in the PACU as well. Technology with seamless integration helps streamline processes, reduce human error, and ensure that critical information is available when needed most. Features such as an intuitive user interface and customizable configurations allow nurses to adapt the technology to specific patient requirements, further enhancing patient-centric care.
\r\nEnhanced connectivity across monitoring devices also plays a pivotal role in PACU safety. Systems capable of facilitating continuous data flow and interoperability with Electronic Health Records (EHRs) ensure that all relevant patient information is up-to-date and accessible. Interoperability supports better coordination and communication among medical teams, making it easier to track the patient’s status throughout the continuum of care.
\r\n
Reliable patient monitoring technology is integral to enhancing safety in the PACU. In this specialized care unit, PACU nurses must have access to accurate, real-time data to make rapid, informed decisions and ensure high standards of patient care and safety. As alarm fatigue continues to be an ongoing concern in critical care departments, devices that feature smart alarms to minimize alarm fatigue help PACU nurses distinguish between false and actionable alerts, keeping the focus on actual patient needs.
Patient monitoring systems that easily integrate into existing hospital workflows can help enhance patient care in the PACU as well. Technology with seamless integration helps streamline processes, reduce human error, and ensure that critical information is available when needed most. Features such as an intuitive user interface and customizable configurations allow nurses to adapt the technology to specific patient requirements, further enhancing patient-centric care.
Enhanced connectivity across monitoring devices also plays a pivotal role in PACU safety. Systems capable of facilitating continuous data flow and interoperability with Electronic Health Records (EHRs) ensure that all relevant patient information is up-to-date and accessible. Interoperability supports better coordination and communication among medical teams, making it easier to track the patient’s status throughout the continuum of care.

How Patient Monitoring Technology Can Alleviate Staffing Challenges in the PACU
As a result, PACU nurses are required to be flexible throughout their shifts, but this can lead to fatigue, which can ultimately impact patient safety. Patient monitoring technology that offers a universal interface, automated vital signs capture, and parameters to help combat alarm fatigue, can help PACU nurses work more efficiently, especially when staffing challenges persist.
\r\n
PACU nurses typically care for one or two patients at a time to provide the personalized and routine care required in this setting. A 2013 study demonstrated that nursing workloads in the PACU are influenced by the magnitude of the surgery, individual patient acuity, and length of stay.4 As clinical priorities change, PACU nurses may have to shift gears and tend to one patient whose condition is worsening during phase I of their stay.
As a result, PACU nurses are required to be flexible throughout their shifts, but this can lead to fatigue, which can ultimately impact patient safety. Patient monitoring technology that offers a universal interface, automated vital signs capture, and parameters to help combat alarm fatigue, can help PACU nurses work more efficiently, especially when staffing challenges persist.

Conclusion
Efficient patient monitoring in the PACU is essential for patient safety and care during this phase of recovery. By utilizing advanced monitoring technologies, adhering to best practices, and staying current on the latest trends and innovations, healthcare professionals are taking appropriate steps to ensure optimized patient care and outcomes in the critical postoperative phase and alleviate the stresses they face while caring for patients in the PACU environment.
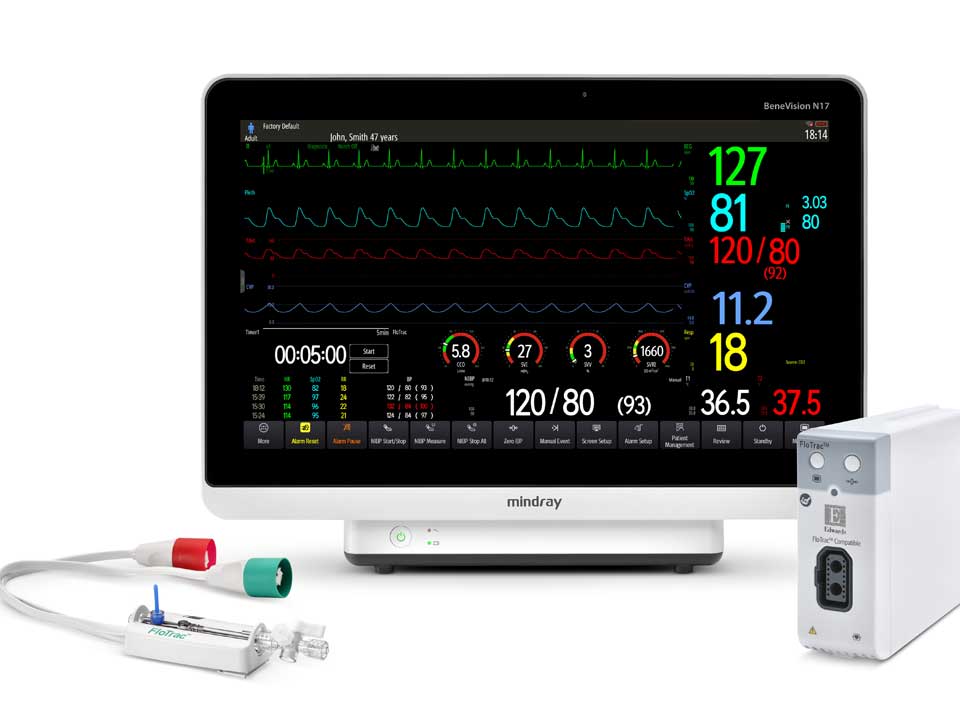
The Mindray Difference in Patient Monitoring
At Mindray, we understand the need for individualized and efficient care in the PACU environment. Our intuitive patient monitoring solutions help streamline patient care and ensure clinicians have quick access to comprehensive and meaningful data at the bedside and beyond. Mindray’s BeneVision N-Series Patient Monitors, now Integrated with Edwards FloTrac™ sensor, offer an advanced monitoring solution that provides clinicians with greater insights into a patient’s hemodynamic instability. The N-Series is the first monitoring platform that integrates directly with the FloTrac™ sensor on the market today. The Mindray VS 9 Vital Signs Monitor is designed to be connected so clinicians can send vital signs at the POC, simplifying workflow, improving efficiencies, and reducing errors.
\r\n\r\n
[1] Luckowski, Amy PhD, RN, CCRN, CNE. Safety priorities in the PACU. Nursing 49(4):p 62-65, April 2019. | DOI: 10.1097/01.NURSE.0000554246.74635.e0
\r\n[2] Pusey-Reid, Eleonor DNP, MEd, RN, CCRN. Patient readiness for PACU discharge. Nursing Critical Care 13(5):p 31-34, September 2018. | DOI: 10.1097/01.CCN.0000544399.76592.be
\r\n[3] Pusey-Reid, Eleonor DNP, MEd, RN, CCRN. Patient readiness for PACU discharge. Nursing Critical Care 13(5):p 31-34, September 2018. | DOI: 10.1097/01.CCN.0000544399.76592.be
\r\n[4] Luckowski, Amy PhD, RN, CCRN, CNE. Safety priorities in the PACU. Nursing 49(4):p 62-65, April 2019. | DOI: 10.1097/01.NURSE.0000554246.74635.e0
\r\n"}}" id="text-fa0aafa920" class="8f00b2 cmp-text">References:
[1] Luckowski, Amy PhD, RN, CCRN, CNE. Safety priorities in the PACU. Nursing 49(4):p 62-65, April 2019. | DOI: 10.1097/01.NURSE.0000554246.74635.e0
[2] Pusey-Reid, Eleonor DNP, MEd, RN, CCRN. Patient readiness for PACU discharge. Nursing Critical Care 13(5):p 31-34, September 2018. | DOI: 10.1097/01.CCN.0000544399.76592.be
[3] Pusey-Reid, Eleonor DNP, MEd, RN, CCRN. Patient readiness for PACU discharge. Nursing Critical Care 13(5):p 31-34, September 2018. | DOI: 10.1097/01.CCN.0000544399.76592.be
[4] Luckowski, Amy PhD, RN, CCRN, CNE. Safety priorities in the PACU. Nursing 49(4):p 62-65, April 2019. | DOI: 10.1097/01.NURSE.0000554246.74635.e0